As women age, the number and quality of their eggs (oocytes) naturally declines. In fact, the ovaries are populated with the highest number of eggs at about 28 weeks gestations – months before birth occurs. Over time, eggs are lost through a normal process called atresia. By the time females experience their first menstrual period, the majority of their total egg count is depleted from about 6 million to several hundred thousand. When menopause occurs only about 1000 total eggs remain.
The age of each patient, their social habits (smoking for example), medical and surgical history, and most importantly their “genes” determines their overall egg health. Although fertility specialists don’t always agree, most of us define egg health (technically called ovarian reserve) as a combination of potential egg quantity (How many eggs can be obtained in an IVF cycle, for example?) and egg quality (How likely will the eggs combine with the sperm to produce a genetically normal embryo and then a healthy baby?).
Egg health can be estimated in a number of ways and in general, more than one method should be applied to each patient. Overall, maternal age continues to be the best predictor of each couple’s chances of success. However, within age groups, significant variations in ovarian reserve do occur – not all 38 year old females have the same chance of success with a given fertility treatment each month. Hormone testing and ultrasound evaluation are the most practical and accurate methods for the estimation of each patient’s egg health. Anti-Mullerian hormone (AMH), which is relatively stable throughout the menstrual cycle, has the best performance characteristics for the prediction of live birth and is convenient for patients since it can be drawn at any time. FSH (follicle stimulating hormone) and estrogen levels are also hormone tests used to estimate egg health.
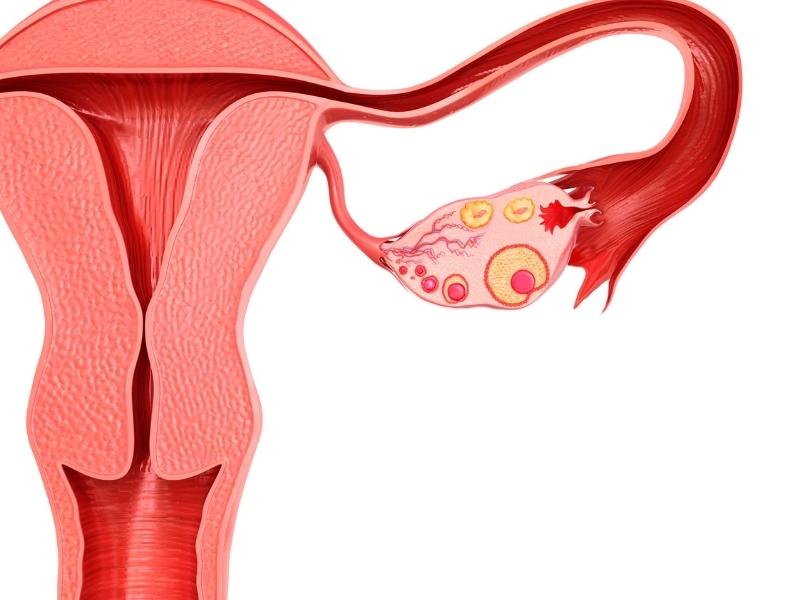
Ultrasound is also often used to evaluate ovarian reserve. Ultrasound visualization of each ovary allows small, early follicles (each small follicle contains an egg) to be counted. This is often referred to an antral or resting follicle count. Higher numbers usually indicate overall better egg health and a more significant potential response to fertility treatment(s). Please, be aware that the antral follicle count is reflective of your egg health and does not accurately predict the exact number of eggs that remain in each ovary (an antral follicle count of 12 does NOT mean only 12 eggs remain to achieve pregnancy).
Patients with diminished ovarian reserve or poor egg health are often treated with medications that “encourage” the ovaries to produce more than one egg. IVF, for example, utilizes injectable medications that act on each ovary to facilitate the aspiration (collection) of multiple eggs at the time of egg retrieval. IVF also allows for the genetic testing of each embryo to determine that it has the correct number of chromosomes. Some supplemental vitamins are being studied with regard to their potential effect on egg health. Androgens such as DHEA and testosterone as well as the vitamin CoQ10 may help “fortity” the eggs within the ovaries.
Measures of ovarian reserve and egg health are not perfect but they are useful for determining why some couples struggle to conceive, counseling patients regarding treatment outcomes, and designing optimized, cost-effective and safe treatment plans.
Contact: Appt or Ask Questions at 303-794-0045 or Email Us on our Contact Us page